Olivia Shaw asked medico-legal experts for their comments on a patient’s journey through the health system with potential cauda equina symptoms.
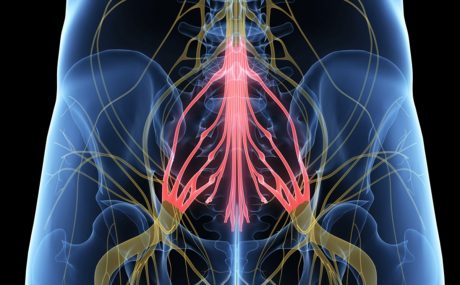
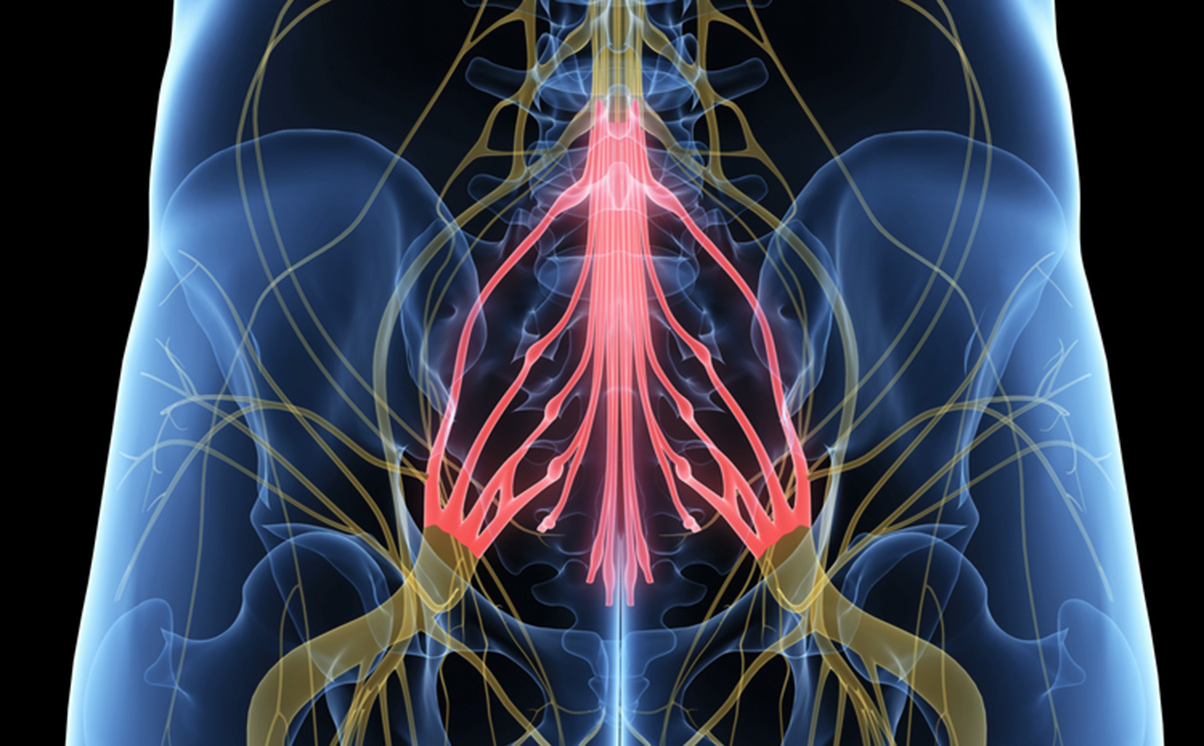
Cauda equina syndrome occurs when the nerve roots in the lumbar spine are compressed, cutting off sensation and movement. Nerve roots that control the function of the bladder and bowel are especially vulnerable to damage.
The first port of call for most patients with symptoms would be a visit to their local GP practice. A patient may then be referred for further examination at their local accident and emergency department (A&E), and if cauda equina syndrome is diagnosed, an operation is carried out by neurosurgeons.
Thank you to Dr Ingram (GP), Dr Kennedy (A&E consultant), Mr Radatz (consultant neurosurgeon) and Robert Dransfield, a partner at Stewarts, for their helpful advice about cauda equina syndrome.
Dr Ingram, back pain is a common complaint at the GP. How do you differentiate this from potential cauda equina syndrome? What are the red flag symptoms that would trigger a referral to the hospital? Do you need more than one red flag?
Back pain is such a common presentation in general practice that all GPs will be familiar with it in most of its forms. However, it is the rare, serious presentations that can catch you out, be it cauda equine, abscess or infection.
As a result, GPs will be looking for alerting features that warrant more analysis or action. Progressive symptoms, the onset of neurology such as pins and needles numbness, weakness, bilateral symptoms and nighttime symptoms, all suggest potential problems.
However, the development of bladder or bowel change, alteration in sensation in the ’saddle’ area (does it feel normal when you wipe yourself on the loo?), or rapidly progressive changes in neurological symptoms all need admission to hospital for assessment.
Quite simply, however many times symptoms turn out NOT to be cauda equine (and in 90% of the admissions, that is quoted to be the case), just saving 1 in 10 of such suspicious cases from a lifetime of spinal injury means that the symptoms above need emergency action from the GP.
Dr Kennedy, what are the red flag symptoms you look for in a patient who attends A&E with potential cauda equina? What investigations are done, and what is the course of action taken?
The view from A&E is relatively simple. I would take a full history and examination of the lower limbs, including checking perianal sensation and anal tone. When anyone attends A&E with back pain (non-traumatic), cauda equina is the diagnosis we need to rule out.
If the patient complains of the following symptoms, then I am either going to refer or arrange an MRI scan for the patient and act on the result:
- Pain going down both legs (bilateral sciatica)
- Difficulty passing urine, urinary retention or incontinence, or altered/abnormal sensation when passing urine
- Weakness and/or altered sensation in both legs, especially if progressive
- Altered perianal or genital sensation
- Altered anal sensation, anal control, feeling of the need to defecate, or
- New impotence or priapism.
Even if this is negative, we refer the following patients and carry out blood tests on them:
- under-20s
- over 55s
- patients with weight loss,
- patients with systemic illness
- patients with pyrexia
- corticosteroid users
- patients with osteoporosis
- patients with HIV, and
- intravenous drug users
For any patient with a history of recent trauma that did not have the above symptoms beforehand but now does or developed these symptoms or other neurology, we would send them for a CT scan and then refer them for an MRI scan, or MRI and then refer to a neurosurgeon.
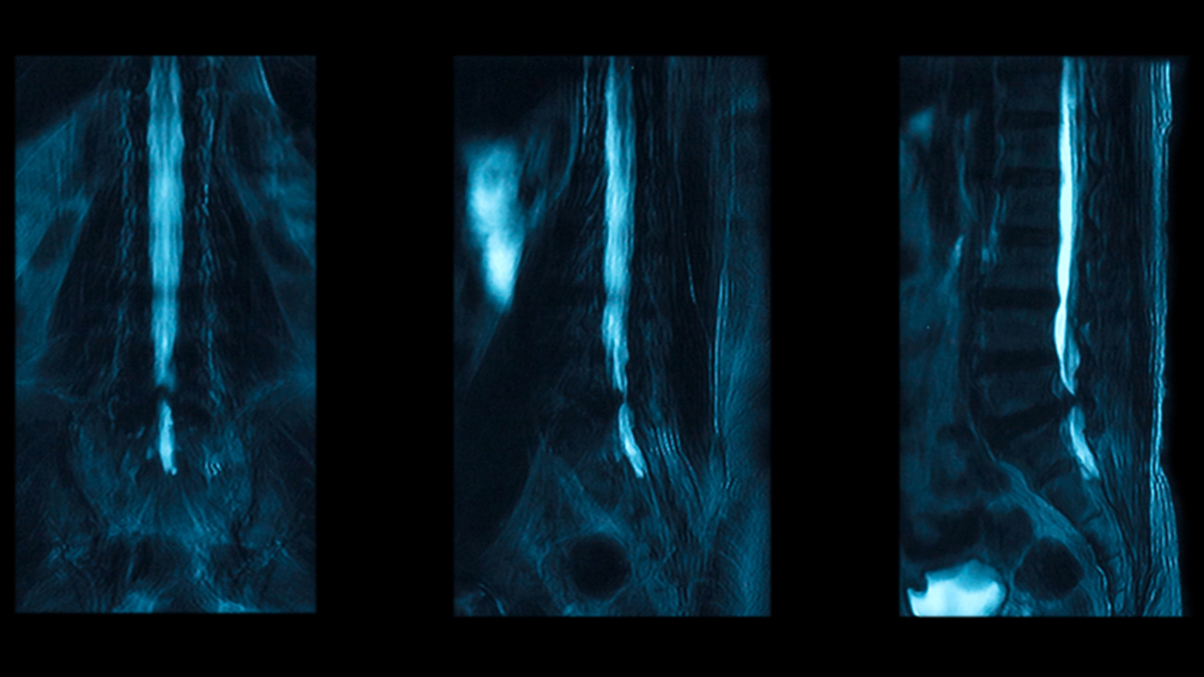
Nobody goes home with non-traumatic back pain until cauda equina/cord compression has been excluded either through history and exam, or history, exam and MRI scan.
Mr Radatz, when a patient reaches you with cauda equina syndrome, how do you identify how progressed their symptoms are? What is the watershed between a good and bad recovery?
Cauda equina syndrome can present with varying symptoms typically associated with an acute presentation of back and leg pain. Most commonly, it is caused by an acute lumbar disc prolapse causing compression of the lumbar sacral nerve roots.
The presentation depends on the level of this disc prolapse and the involvement of different roots. Sensory impairment and weakness are typically present but do not have to be the dominating feature. A saddle sensory deficit, subjective even or objective, are typical features and often lead to urinary symptoms. Here, it is important to acknowledge that it is the patient’s difficulty or inability to urinate normally or feel and control urine flow. Often, the patient might just voice that it does not feel normal. This should be good enough to raise concern and lead to emergency diagnostic, an MRI of the spine being the diagnostic test required.
The level of deficit indicates the level of progression. Red flag signs are there to raise concern before a more permanent deficit will develop. The time of the diagnosis and emergency treatment are essential. Once a patient is insensate, which means anaesthetic and double incontinent, the outcome is typically poor.
It is, therefore, crucial that patients are identified early before such deep deficit develops. Early diagnosis and surgical management will typically facilitate a full or near full recovery.
Robert, at what stage would a patient come to you for advice on their treatment of cauda equina? How often do you see these types of cases, and what can you do to help?
I am generally contacted further to a poor outcome following hospital treatment. I find that either there were issues with referral or a delay, such that the patient is already upset about their treatment. Quite a few patients contact me because a doctor (usually their surgeon or a clinician post-surgery) advised them that they should have had a different outcome.
For those patients immediately post-injury or in rehabilitation, I can help with non-compensation issues through our pro-bono service. That can range from assistance with debts through to powers of attorney.
In terms of post-injury life, if someone does have a claim, I can advise on the merits and work towards obtaining compensation. If we do have access to interim damages, we can help appoint a case manager, set up therapies and assist in helping to rebuild their life post-injury.
You can find further information regarding our expertise, experience and team on our Clinical Negligence pages.
If you require assistance from our team, please contact us.
Subscribe – In order to receive our news straight to your inbox, subscribe here. Our newsletters are sent no more than once a month.